Health equity is a human right
"Evidence suggests that some subgroups are at greater risk for deteriorating mental health than others. A one-size-fits-all approach to service models is not effective."
Dr. Kwame McKenzie
Health equity is the goal for many health systems.
It uses information and data to help the system use resources efficiently by ensuring that the people with the most need get the most services. It allows individuals to reach their full health potential in a fair and appropriate way. It helps ensure that the health care system meets people’s needs regardless of their background (Health Quality Ontario, 2017).
Uneven exposure to the social determinants of health is a contributing factor to health inequities among sub-populations. Reducing disparities in health care requires understanding what causes these disparities, along with recognizing what immigrants and refugees need to settle, integrate and thrive effectively (Ontario Ministry of Health and Long-Term Care [MOHLTC], 2012). Decreasing the risk of illness and increasing the chances of recovery by a focus on the social determinants of health can improve health equity.
What makes Canadians Sick?
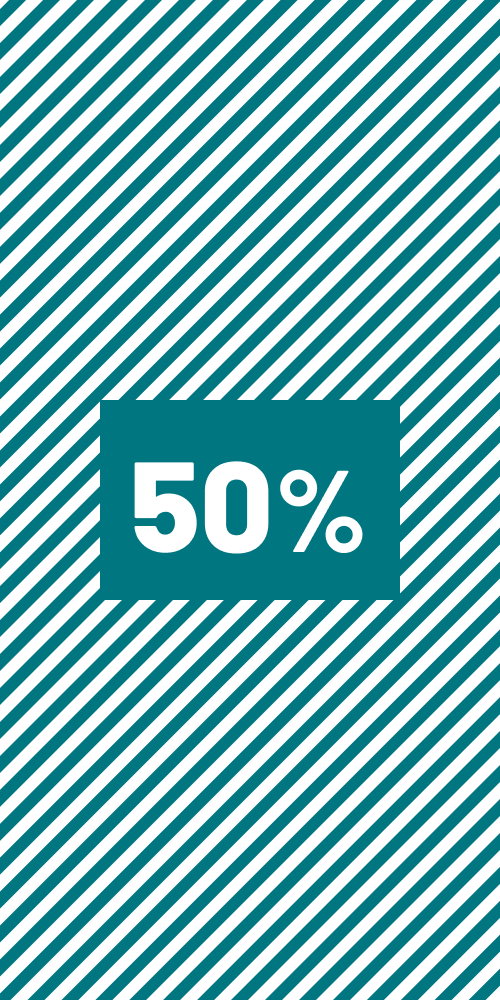
As the graph below illustrates, social factors are very influential; they can account for about half the variation in a person's health status.
These determinants affect all groups in Canada, both immigrant and non-immigrant. The factors commonly recognized as the social determinants that affect Canadians' lives are:
- Income
- Early childhood development
- Disability
- Education
- Social exclusion
- Social safety net
- Gender
- Employment/working conditions
- Race
- Aboriginal status
- Safe and nutritious food
- Housing/homelessness
- Community belonging

- Access to health care
- Health care system
- Wait times
- Biology
- Genetics

- Air quality
- Civic infrastructure
Health equity can be improved by improving service access, the experience that patients have and outcomes from services. It can break the vicious cycle that some immigrant groups say occurs in Canada. They say that when immigrant and racialized populations experience poor care or perceive that they will experience discrimination, it reduces their interest in seeking care within the health care system. As a result, they may turn to non-medical services to address their mental health concerns or their illness will deteriorate leading to more use of emergency services, criminal justice system services and more dramatic and coercive interactions with mental health services. This leads to further reluctance to use services. (Mental Health Commission of Canada [MHCC], 2019).
Ensuring appropriate, timely access to mental health services that are capable of offering sensitive equitable care can improve outcomes for all. If this is not done it can have a negative effect on the health of marginalized communities. Outcomes are improved when the settlement sector and mental health system work together (MOHLTC, 2012).
Integrating health equity metrics and objectives into operational and strategic plans can accomplish two goals: It can foster a common understanding among boards and senior leadership; and it can help leaders take responsibility for improving equity for service users and communities. This demonstrates a concrete commitment to health equity at the leadership level and ensures indicators are analyzed through an equitable lens (Alliance for Healthier Communities, n.d).
Services that are accessible, equitable, person-centred and focused on client needs can lead to trust and confidence in the services being offered and build clients’ ability to take control and manage their own health. This inclusion and increased trust encourage help-seeking behaviours, which can lead to more beneficial health behaviours and a higher quality of life (Alliance for Healthier Communities, n.d).